What is a feeding tube?
A feeding tube delivers a nutrient feed directly into the stomach or intestine. This allows an adult with a muscle-weakening condition to meet their nutritional needs without chewing or swallowing food. They are quite common in adults with muscle-weakening conditions.
Why might you need one?
There are three main reasons why adults with muscle-weakening conditions may require a feeding tube:
1. Recurrent chest infections from aspiration (food getting into the lungs due to swallowing difficulties)
2. Under-nutrition and weight loss which doesn’t respond to swallowing and nutrition strategies
3. Patient preference – if a patient opts to install a feeding tube before severe problems develop. This might be where eating is difficult or they are at risk of aspiration or malnutrition
Types of feeding tube:
Feeding tubes come in three different varieties:
- A nasogastric tube goes up the nose and down the throat to the stomach. These tubes are typically only used on a temporary basis. They can provide necessary nutrients while fighting an infection, or while waiting for a more permanent feeding tube.
- A gastrostomy tube is a tube that goes through the skin directly into the stomach. A hole, or stoma, is made in your skin. These can either be a percutaneous endoscopic gastrostomy (PEG) or a
radiologically inserted gastrostomy (RIG), which refers to how they are inserted:- With a PEG tube, an endoscope (camera) is inserted via the mouth and down into the stomach. This helps the doctor locate an insertion site for the tube. Following an incision in the skin, the PEG tube passes through the mouth, down into the stomach and out through the incision. The doctor then secures it in place. A PEG is usually the preferred method of tube insertion when possible.
- A RIG tube uses X-rays to locate the insertion site for the tube. An incision is made in the skin and the tube is passed through from the outside and secured in place. RIGs may be required where an endoscope/PEG tube cannot safely be passed down the throat.
- A gastrostomy tube can also have an extension into the intestine, allowing it to work like a jejunostomy tube
- A percutaneous endoscopic jejonostomy (PEJ) or jejonostomy (JEJ tube) goes through the skin directly into the jejunem. This is beginning of the small intestine. This may be required if an individual has problems feeding into their stomach.
“When I got my feeding tube my doctor explained the procedure to me and I had it done two weeks later. Honestly, the pain was a lot less than I expected. Without it there is no way I could eat enough by mouth and it’s really great for taking medicine. In 10 years I’ve never had any problems with it”.
Tim, USA
Considerations for a gastrostomy tube

Gastrostomy insertion should ideally take place in a multidisciplinary specialist centre. It is best if you see a specialist gastroenterologist or radiologist experienced with patients with neuromuscular disorders. The decision to insert a tube is a joint one between the patient and their multidisciplinary team. Anaesthetics used for the procedure depend on local practice. They may involve local or general anaesthetic or sedation delivered via IV.
An echocardiogram and electrocardiogram should be done before any general anaesthesia. They should also be done before any conscious sedation, regional anaesthesia or local anaesthesia. This is even more important if previous echocardiograms have shown reduced cardiac function or were undertaken over one year previously. If an individual is on steroids, consideration needs to be given to steroid cover over the period of surgery. This is because you can develop adrenal insufficiency on steroids.
The following drugs should always be avoided during any procedure:
- Inhalational anaesthetic agents, such as halothane and isoflurane. If anaesthetic is required it should be delivered exclusively by intravenous injection due to rhabdomyolysis. Rhabdomyolysis complications are frequently confused with malignant hyperthermia
- Depolarising muscle relaxants, such as suxamethonium chloride, must not be used due to the risk of fatal reactions.
- Postoperative anticoagulation with heparin and/or aspirin is inappropriate and should be stopped pre-procedure
Non-invasively assisted ventilation and the use of a cough assist is recommended during and after procedure for patients with significant respiratory-muscle weakness. Adults with DMD not currently using NIV or cough assist should be trained in their use prior to any surgery.
(DMD Care Considerations Working Group, 2018)
“I definitely want to eat as long as I can by mouth by any means necessary, since I really love and enjoy not just eating, but food in general and love cooking with the help of my PCAs. I’m a foodie. But if my health declines to the point that I can no longer safely eat by mouth, then I would want a feeding tube, because I’m a huge fan of staying alive”.
Petr, 21
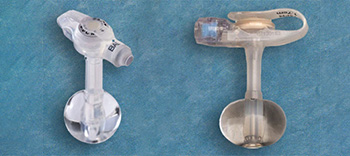
What does it look like?
There are different types of gastrostomy tubes. Some such as low- profile devices sit flush with the stomach. However, gastrostomy tubes are discreet and are not noticeable under the clothes.
Can you still eat?
Getting a feeding tube doesn’t necessarily mean that you won’t be able to eat or drink normally. Many adults use a feeding tube to get most of their nutrition and make sure they maintain a healthy weight, but still eat and drink for comfort or when they feel like it. Having a feeding tube removes the pressure on the adult to always make sure they are eating enough and getting a healthy diet. Other adults only use the feeding tube when they are ill or for taking medication.
How are you fed through it?

Specially prepared liquid feeds, which contain all the nutrients the adult needs, are fed into the stomach using the feeding tube. There are different options as to how and when the feed is administered depending on the individual’s preferences.
Some people prefer the feed to be delivered by a pump, which can be done overnight or during the day, at different speeds depending on what is best tolerated. Some people prefer the feed to be delivered at regular mealtimes, using a syringe to insert the food in portions throughout the day. This is known as bolus feeding.
Are there different types of feed?
Standard feeds are designed to meet the complete nutritional requirements of an adult. Many different companies make feeds so there can be small variations in products depending on the company; but essentially feeds are very similar. There are also specialised feeds to meet different nutritional needs (e.g. to provide more calories in less fluid, or with increased fibre).
How do you take care of it?
It is important to keep the feeding tube site clean at all times, to avoid any infections and to avoid excess granulation tissue (tissue that forms on wound surfaces during the healing process). It can be useful to rotate the tube a couple of times each day to prevent it sticking to the stomach wall. The site needs to be kept dry, after being cleaned, to prevent soreness, redness and becoming itchy. Occasional mild dampness on the skin is normal, but if heavily or regularly soiled this should be mentioned to a healthcare professional. Care must be taken to prevent the feeding tube from being caught or pulled during hoisting and other movements (e.g. moving & handling, physio, sex).
If you have a RIG tube, this is held in place by an inflated balloon of water, so a little more care might be needed. If you have a PEG tube, this is secured by a button inside the stomach, and is rarely dislodged, but pulling the tube could still cause trauma and/or bleeding.It can be useful to tape the tube to the skin to keep it out of the way, but be sure to use dressings and tape that are not going to irritate your skin.
“In my routine, I clean the tube site twice a day, in the morning during my bath/shower with soap and water, and then in the evening with saline water and gauze. To hold the tube in place and
Tyran, UK
protect it, I use two circular cotton wool pads as a small dressing, with an incision to the centre. This is placed around the tube to protect the skin in this area. Gauze is then used as padding underneath the tube and secured with Hypafix tape”.
What can go wrong and how to deal with it
It is essential to put a plan in place with your nutrition team if the tube accidentally falls out or migrates. If the tube falls out, the stoma will close within a few hours so it is important to act quickly. If it is a bumper- retained tube and the tract is kept open, a local hospital can change the tube without needing a procedure. However, if it is a balloon-retained gastrostomy (i.e. held in place with a water filled balloon), a spare balloon tube should be kept at home as these are changed regularly at home.
“It is not unusual for you to experience some slight seeping around the PEG site, even on a good day. Normally anything spilt on your skin can be easily wiped off without causing much irritation, however when the fluid is slightly corrosive and continually leaking in small amounts it can cause some irritation. In my experience it is a bit of a nightmare to treat this after it begins to get sore, what I find helps is to get a decent barrier cream applied to my skin on a morning, night or whenever it begins to feel itchy”.
Robert, UK
“Before using a silicone g-tube I used flimsy rubber ones and had a lot of problems with clogging. Since I’ve been using silicone for the last several years it hasn’t clogged even once”.
Pacien, US


